The Silver Lining of the New Skilled Nursing Facility Staffing Rule for Medicare and Medicaid Reimbursement
In another milestone move toward value-based care, the Centers for Medicare and Medicaid Services (CMS) finalized a new Skilled Nursing Facility (SNF) minimum staffing rule on April 22, 2024. This rule is expected to cost the SNF care setting an additional $6.5 billion a year.
This cost includes hiring more than 77,000 Certified Nurse Aides (CNAs) and 24,000 Registered Nurses (RNs). Until that’s possible, nearly 25% of SNF nursing home residents— that's 290,000 people — are at risk of being displaced.
Key Takeaways
- The Centers for Medicare and Medicaid Services (CMS) finalized a new Skilled Nursing Facility (SNF) minimum staffing rule on April 22, 2024.
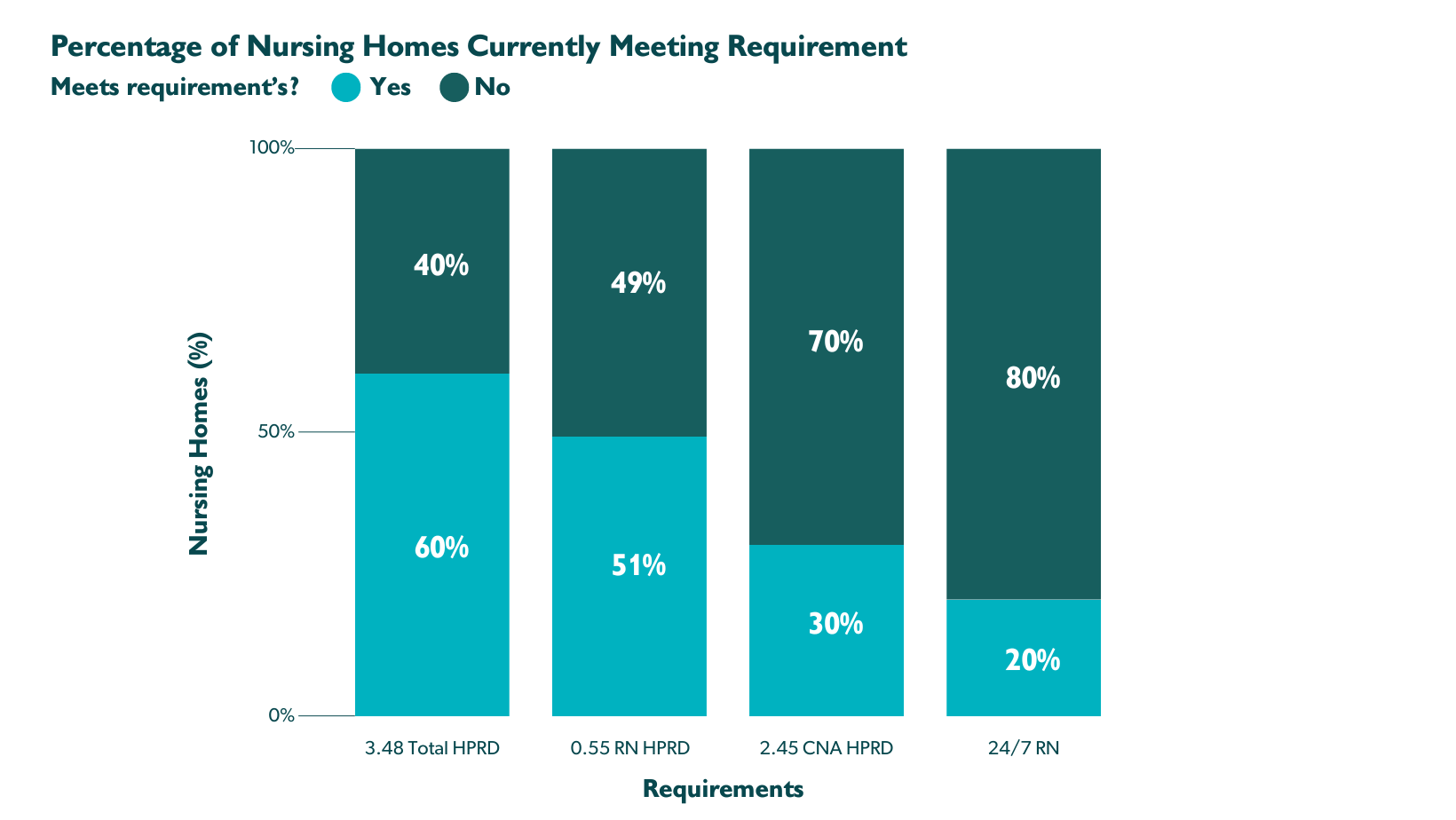
- The rule requires 3.48 nursing staff hours total per resident per day (HPRD).
- The rule is expected to cost the SNF care setting an additional $6.5 billion annually.
- SNFs have three years to comply, and rural facilities have an additional two years (five total).
- To prepare for the shift, SNFs can pursue financial, workforce, technology and advocacy planning that may open up new reimbursement and funding opportunities.
Minimum Staffing Rule
3.48 nursing staff hours total per resident per day (HPRD)
> 2.45 CNA
> .55 RN
RN on site 24/7
Only 6% of SNFs currently comply with these standards.
While the gravity of the situation for SNFs and their nursing home residents is hard to overstate, there are some rays of hope to be aware of.
SNFs Don’t Have to Shift Overnight
SNFs have three years to comply with the minimum staffing rule, and rural facilities have an additional two years for a total of five. For now, you can think of the rule as a roadmap with clear steps towards the destination. You can pursue a hardship exemption, but it will only be considered if you invest in staff recruitment and retention and show proactive steps toward improving your situation.
You Do Have to Update Your Facility Needs Assessment — Soonish
The minimum nurse staffing standards have been added to the Federal Register, and publication is imminent. You’ll have 90 days from the publish date to update your facility needs assessment.
 Strategies for Skilled Nursing Facilities
Strategies for Skilled Nursing Facilities
Explore these strategies for planning and preparing for the new minimum staffing rule:
- Financial planning and cost management
- Workforce planning and recruitment
- Technology time savers
- Advocacy and collaboration
Take a look at your staffing levels and resident needs to identify gaps under the minimum staffing rule. Estimate the cost of covering the gap, including salaries and benefits, and look for new ways to generate funding.
CMS offers incentives for providing value-based care, including the SNF Value-Based Purchasing (SNF VBP) program and the Patient-Driven Patient Model (PDPM).
SNF VBP
CMS withholds 2% of all fee-for-service (FFS) payments to SNFs to fund the incentive program. Then, CMS re-distributes 60% of program funds to SNFs that show achievement or improvement on a single value-based care quality measure: unplanned hospital readmissions within 30 days.
Additional quality measures — and more opportunities to earn incentives — we may see in the next few years include:
- Health-associated infections requiring hospitalization
- Falls leading to major injury
- Nursing staff turnover
- Discharge to community
PDPM
The PDPM model groups Medicare Part A patients into different reimbursement categories based on their:
- Diagnosis
- Functional ability and limitations
- Cognitive impairment
- Co-occurring conditions
- Level of care needed after SNF discharge
While not mandatory yet, the CMS is moving swiftly in this direction.
You can also pursue grants from alternate government funding sources, including:
- U.S. Department of Health and Human Services
- Health Resources and Services Administration (HRSA)
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- Grants.gov

Workforce Planning and Recruitment
Weigh recruitment strategies to help you attract RNs and CNAs such as partnering with nursing schools and participating in career fairs and job boards.
Keep your current staff happy by:
- Providing opportunities for professional development
- Creating a positive, supportive work environment
- Communicating early and often about staffing plans and progress
Technology Time Savers
Investigate technologies that drive quality achievements while saving time and increasing resident satisfaction:
- Data analytics for real-time decision support and outcomes reporting
- Telehealth and remote patient monitoring for increased access to care
- Electronic medical records with digital charting for faster information capture that can be instantly and securely shared
- Automated workflows, including appointment scheduling and appointment reminders, to ease staff burden and smooth patient experience
Advocacy and Collaboration
Stay up to date as developments around the minimum staffing rule unfold and rally support from industry associations and legislatures. Collaborate with Affordable Care Organizations (ACOs) to learn how to advance your value-based care and potentially access ACO-based reimbursement incentives.
 More Help Is on the Way
More Help Is on the Way
In response to SNF workforce shortages, the CMS and HRSA announced an investment of $75 million into a national campaign to help recruit people into nursing home careers. The campaign includes opportunities for scholarships and tuition reimbursements.
Remembering It’s About the Residents
While the new minimum nurse staffing standards are expected to cause hardships for nursing homes and residents in the short term, the long-term goal is to provide residents with better care, keeping them safer and out of the hospital.
With more nurses on staff, residents get more attention, including assistance with daily living activities:
- Bathing
- Dressing
- Toileting
This can improve residents’ comfort and well-being.
More RN attention can also mean improved safety, with more accurate medication administration, better pain management and quicker response to calls, reducing resident anxiety and frustration. All these resident benefits can drive lower hospital readmissions.
Consider the residents’ caregivers, too
What do your residents’ caregivers know about the new minimum staffing rule? Absolutely nothing or just enough to be worried?
It’s time for some open communication. You can hold an information session to explain the new rule, its purpose, and the potential impact on resident care. Bring along educational materials — feel free to use the information in this article — and come prepared with a list of community resources and support groups.
Accentuate the positive, highlighting the long-term benefits of the change, including better quality of life and care.

How to Talk to Your Staff About the Changes
Like resident caregivers, your staff likely has concerns, whether they’re expressing them or not. If you haven’t already, schedule a meeting to hear them out.
Come prepared with information about the new rule, acknowledge the challenges and highlight the benefits as you would with residents’ caregivers.
During the meeting, encourage everyone to ask questions and offer ideas. Emphasize the importance of collaboration for a smooth transition and steer the conversation toward solutions. Resist the temptation to make promises you can’t keep. It’s OK if you can’t answer a question, but make sure to follow up.
Above all, thank your staff for their dedication and hard work and give them your commitment to support them.
Frequently Asked Questions
What are the new staffing requirements for skilled nursing facilities?
Skilled nursing facilities are required to have a 24-hour registered nurse presence and meet minimum staffing standards, which will be phased in over three years for non-rural facilities. CMS mandates this rule to improve the quality of care in these facilities.
What are the financial implications of the new rule?
The new rule is expected to lead to an extra industry-wide cost of roughly $6.5 billion annually. This will have significant financial implications for skilled nursing facilities.
What strategies can help skilled nursing facilities meet the new staffing minimum?
Explore these strategies for planning and preparing for the new minimum staffing rule:
- Financial planning and cost management
- Workforce planning and recruitment
- Technology time savers
- Advocacy and collaboration
How can minimum nurse staffing standards help nursing home residents?
With more nurses on staff, residents get more attention, including:
- Assistance with daily activities
- More accurate medication administration
- Better pain management
- Quicker response to calls
- Lower resident anxiety and frustration
- Fewer hospital readmissions
How can you address residents’ caregiver concerns?
Hold an information session to explain the new rule, its purpose and the potential impact on resident care. Bring educational materials and come prepared with a list of community resources and support groups. Accentuate the positive, highlighting the long-term benefits of the change, including better quality of life and care.
How can you help your staff deal with the changes?
Set up a meeting and come prepared with information about the new rule. Acknowledge the challenges and highlight the benefits.
During the meeting, encourage everyone to ask questions and offer ideas. Emphasize the importance of collaboration for a smooth transition and steer the conversation toward solutions. Resist the temptation to make promises you can’t keep. It’s OK if you can’t answer a question but be sure to follow up.
Above all, thank your staff for their dedication and hard work and give them your commitment to support them.