Many skilled nursing facilities are winning at value-based care — and the reimbursement incentives that come with it — by using AI to:
- Predict resident needs
- Enhance operational workflows
- Comply with regulations
- Raise the quality of care
Key Takeaways
- Predictive analytics brings the power of big data and machine learning to improve accuracy, streamline care delivery and personalize treatment plans for better healthcare outcomes.
- AI makes operations more efficient by streamlining day-to-day tasks through automation.
- AI can guide you as you navigate the complicated and ever-evolving landscape of regulatory compliance and open up new Centers for Medicare & Medicaid Services (CMS) reimbursement opportunities.
- AI’s innovations in mental health and well-being are transforming skilled nursing facilities, seamlessly merging technology with human care to provide a more nurturing, supportive environment for both residents and staff.
- AI can help you take steps toward compliance with the new CMS minimum staffing rule by helping optimize staffing and increase the value of care.
 Enhancing patient outcomes with AI-driven predictive analytics
Enhancing patient outcomes with AI-driven predictive analytics
Predictive analytics is one of the most powerful AI applications. It brings the power of big data and machine learning to improve accuracy, streamline care delivery and personalize treatment plans for better healthcare outcomes. Skilled nursing facilities are using predictive analytics to:
- Predict risks of illness and injury
- Take action sooner
- Make informed decisions based on each patient’s unique healthcare needs
Predictive analytics enables skilled nursing facilities to see patterns and identify trends before potential risks become real emergencies. It brings clarity to complex healthcare delivery processes and surfaces individual care needs, currently and in the future.
Streamlining operations: AI in skilled nursing facility management
Better care and easier care. What’s not to love about AI in skilled nursing facilities? AI makes operations more efficient by streamlining day-to-day tasks through these common automations:
- Chatbots that handle routine questions
- Appointment scheduling and reminders
- Staff scheduling
- Workflow and next-step coordination
- Compliance reporting
The efficiency gains make everyone happy — residents, staff and the Centers for Medicare & Medicaid Services (CMS).
Facilitating real-time communication
Through secure messaging tools, AI can keep everyone on the same (digital) page, including:
- SNF staff
- External healthcare providers
- Community partners
- Residents
- Residents’ caregivers
An especially popular AI application in skilled nursing facilities is a virtual assistant with speech recognition that:
- Answers routine resident and caregiver questions
- Sends medication reminders
- Schedules appointments
- Tracks symptoms
This makes on-call responsibilities more manageable for healthcare providers while increasing resident satisfaction.
 Applying AI to regulatory compliance and quality measures
Applying AI to regulatory compliance and quality measures
AI can guide you as you navigate the complicated and ever-evolving landscape of regulatory compliance. It can track and analyze compliance data related to resident care, medication administration and staffing levels so you always know where you stand. AI can also alert you to gaps before they become issues and drive improvements in quality and clinical outcomes that may open up more CMS reimbursement opportunities.
Two examples are the SNF Value-Based Purchasing (SNF VBP) program and the Patient-Driven Patient Model (PDPM).
SNF VBP
CMS withholds 2% of all fee-for-service (FFS) payments to SNFs to fund the incentive program.
CMS then re-distributes 60% of program funds to SNFs who show achievement or improvement on a single value-based care quality measure: unplanned hospital readmissions within 30 days.
Additional quality measures — and more opportunities to earn incentives — we may see in the next few years include:
- Health-associated infections requiring hospitalization
- Falls leading to major injury
- Nursing staff turnover
- Discharge to community
PDPM
The PDPM model groups Medicare Part A patients into different reimbursement categories based on their:
- Diagnosis
- Functional ability and limitations
- Cognitive impairment
- Co-occurring conditions
- Level of care needed after SNF discharge
While not mandatory yet, the CMS is moving swiftly in this direction.
 Addressing healthcare industry standards
Addressing healthcare industry standards
AI isn’t something that it is wise to set and forget. The best AI solutions continuously learn from inclusive and diverse training data to keep up with the latest healthcare standards.
Ongoing AI monitoring and audits are necessary to correct emerging biases and disparities. Due diligence in this area supports high-quality, consistent healthcare delivery.
Healthcare professionals must remain vigilant, ensuring that AI’s development and use in healthcare remain ethical. Integrating AI into healthcare is a continuous process that requires human oversight to ensure that the potential risks are mitigated.
Innovations in mental health and wellbeing through AI
AI’s innovations in mental health and well-being are transforming skilled nursing facilities, seamlessly merging technology with human care to provide a more nurturing, supportive environment for both staff and residents.
Supporting staff mental health
The mental health of skilled nursing facility staff is a critical aspect of the SNF ecosystem. AI tools are at work at many facilities to track signs of staff burnout, improve work satisfaction and promote retention.
AI algorithms can analyze:
- Work schedules
- Communication patterns
- Reported incidents
- Potential signs of stress and depression
Early detection allows staff to seek support before problems escalate.
AI-powered chatbots provide an additional layer of assistance by connecting staff to confidential, around-the-clock access to mental health information and resources. Staff can anonymously discuss their concerns and receive expert recommendations for coping mechanisms, stress management techniques, self-care practices and resilience training.
Peer support is often included where AI matches staff to a buddy facing similar challenges for ongoing support.
Standard mental health screenings can also be administered through AI to give staff a gut check and direct them to appropriate help.
 Getting ahead of the minimum staffing rule with AI
Getting ahead of the minimum staffing rule with AI
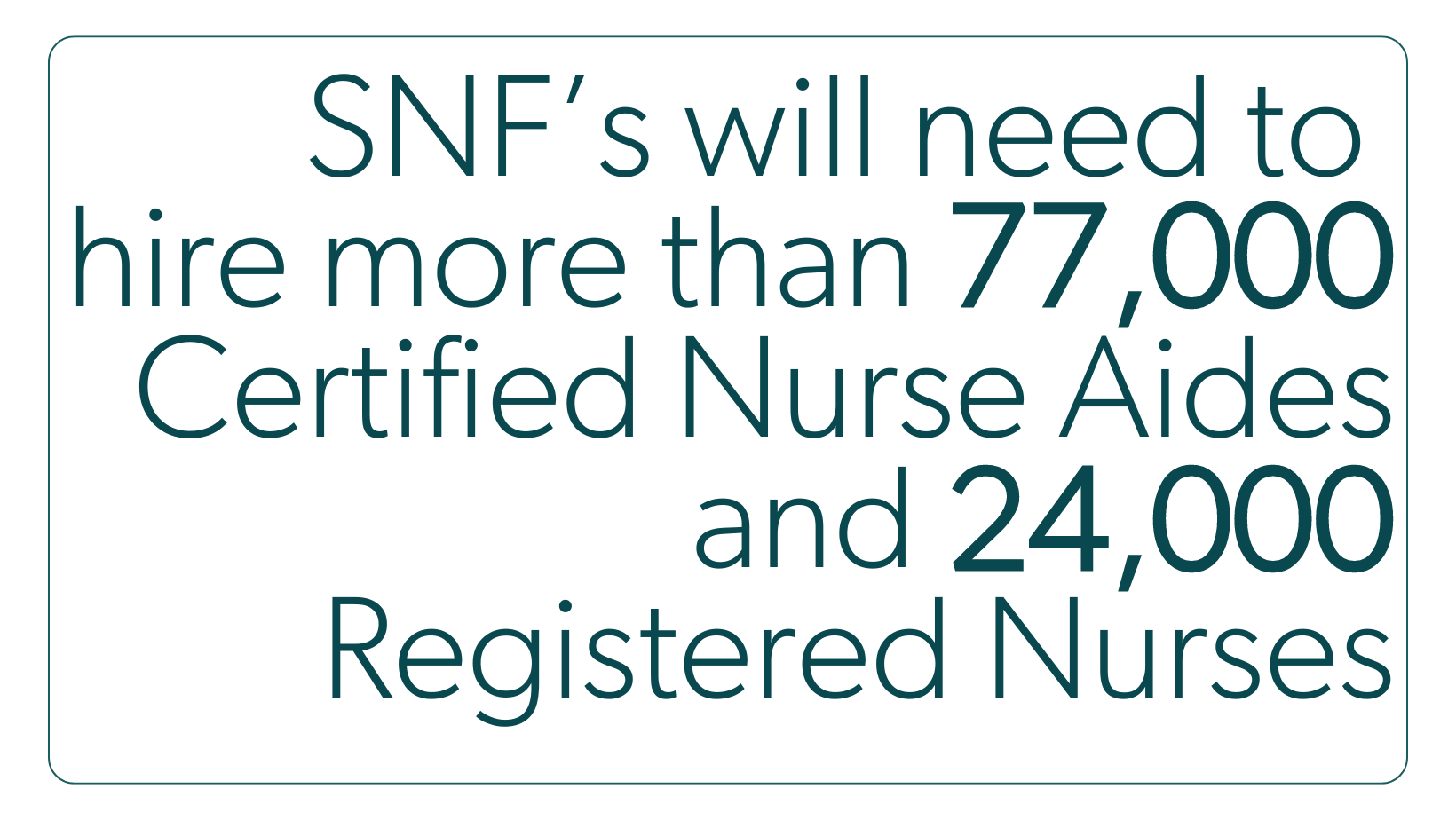
In a milestone move toward value-based care, the CMS finalized a new SNF minimum staffing rule on April 22, 2024, that’s expected to cost the SNF care setting an additional $6.5 billion a year.
This cost includes the need to hire more than 77,000 Certified Nurse Aides (CNAs) and 24,000 Registered Nurses (RNs). Until that’s possible, nearly 25% of SNF nursing home residents — that's 290,000 people — are at risk of being displaced.
SNFs have three years to comply with the minimum staffing rule, and rural facilities have an additional three years for a total of five.
AI can help you take steps toward compliance by helping optimize staffing and increasing the value of care.
 Frequently Asked Questions
Frequently Asked Questions
Why is technology important in value-based care?
Technology enables the use of artificial intelligence and machine learning to analyze patient data and ease administrative burdens for healthcare providers. It helps identify patient healthcare needs and concerns, ultimately supporting the shift toward value-based care models.
What is the role of AI in nursing practice?
AI plays a crucial role in nursing practice by enabling rapid interventions for improved patient outcomes and streamlining administrative tasks to free nurses to focus on patient care.
How does AI-driven predictive analytics improve patient outcomes in skilled nursing facilities?
AI enables early detection of critical medical conditions, improves the accuracy of diagnosis and treatment and supports personalized care plans for better resident care.
Can AI help with the staffing challenges faced by skilled nursing facilities?
Yes. AI is great at this. It can predict staffing needs, manage schedules more efficiently and increase employee retention.
How does AI contribute to care coordination in skilled nursing facilities?
AI contributes to care coordination by automating administrative tasks, facilitating real-time communication among care teams and balancing workloads to prevent healthcare provider burnout.
How can AI prevent staff burnout in skilled nursing facilities?
AI tools can track potential signs of staff burnout like these to improve work satisfaction and promote retention:
- Work schedules
- Communication patterns
- Reported incidents
- Potential signs of stress and depression
Early detection allows staff to seek support before problems escalate.
What are the new staffing requirements for skilled nursing facilities?
Skilled nursing facilities are required to have a 24-hour registered nurse presence and meet minimum staffing standards, which will be phased in over three years for non-rural facilities. CMS mandates this rule to improve the quality of care.
Take a deeper dive into the minimum staffing rule.
What are the financial implications of the new rule?
The new rule is expected to lead to an extra industry-wide cost of roughly $6.5 billion annually. This will have significant financial implications for skilled nursing facilities.
What strategies can help skilled nursing facilities meet the new staffing minimum?
Explore these strategies for preparing for the new minimum staffing rule:
- Financial planning and cost management
- Workforce planning and recruitment
- Technology time savers
- Advocacy and collaboration with community groups and legislators